PTSD Insomnia Treatment: Strategies and Approaches
Post-Traumatic Stress Disorder (PTSD) is a mental health condition that can have a profound impact on a person’s life. One common symptom of PTSD is insomnia, which can exacerbate the effects of the disorder and hinder recovery. Finding effective treatment for PTSD-related insomnia is crucial in improving overall well-being and quality of life.
Understanding PTSD-Related Insomnia
Insomnia is a common symptom experienced by individuals with PTSD. Nightmares, flashbacks, hyperarousal, and anxiety can all contribute to sleep disturbances, making it difficult for individuals to fall asleep or stay asleep throughout the night. Chronic sleep deprivation can worsen symptoms of PTSD, creating a vicious cycle that impacts both physical and mental health.
Treatment Approaches for PTSD-Related Insomnia
There are several strategies and approaches that can be effective in treating insomnia associated with PTSD:
- Cognitive Behavioral Therapy for Insomnia (CBT-I): CBT-I is a structured program that helps individuals identify and change negative thoughts and behaviors that contribute to insomnia. It focuses on improving sleep habits, relaxation techniques, and addressing underlying issues that may be disrupting sleep.
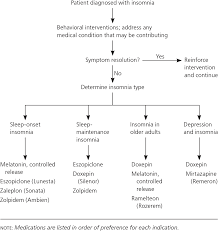
- Medication: In some cases, healthcare providers may prescribe medications to help manage symptoms of insomnia. These medications may include sedatives or antidepressants that can promote better sleep.
- Relaxation Techniques: Practices such as deep breathing exercises, progressive muscle relaxation, mindfulness meditation, and guided imagery can help calm the mind and body before bedtime, making it easier to fall asleep.
- Sleep Hygiene: Establishing a consistent bedtime routine, creating a comfortable sleep environment, limiting screen time before bed, avoiding caffeine and alcohol close to bedtime, and maintaining a regular sleep schedule can all contribute to better sleep quality.
Seeking Professional Help
If you are struggling with PTSD-related insomnia, it is important to seek help from mental health professionals who specialize in trauma-informed care. A qualified therapist or counselor can work with you to develop a personalized treatment plan that addresses your specific needs and challenges.
Remember that recovery from PTSD-related insomnia takes time and patience. By incorporating effective treatment approaches into your daily routine and seeking support from healthcare providers, you can improve your sleep quality and overall well-being as you work towards healing from PTSD.
Understanding and Managing PTSD-Related Insomnia: A Comprehensive Guide to Symptoms, Treatments, and Self-Help Strategies
- What is PTSD-related insomnia?
- How does PTSD contribute to insomnia?
- What are the symptoms of PTSD-related insomnia?
- What treatment options are available for PTSD-related insomnia?
- Is cognitive behavioral therapy effective in treating PTSD-related insomnia?
- Are there medications specifically for treating insomnia in individuals with PTSD?
- What lifestyle changes can help improve sleep quality for individuals with PTSD?
- How can relaxation techniques benefit those experiencing PTSD-related insomnia?
- Should individuals seek professional help for managing PTSD-related insomnia?
What is PTSD-related insomnia?
PTSD-related insomnia refers to the sleep disturbances experienced by individuals with Post-Traumatic Stress Disorder (PTSD). It is a common symptom characterized by difficulty falling asleep, staying asleep, or experiencing restful sleep due to the effects of trauma. Factors such as nightmares, flashbacks, hyperarousal, and anxiety associated with PTSD can significantly disrupt the sleep cycle and lead to chronic sleep deprivation. Addressing PTSD-related insomnia is essential in managing the overall impact of PTSD on an individual’s well-being and quality of life.
How does PTSD contribute to insomnia?
Post-Traumatic Stress Disorder (PTSD) can contribute to insomnia through a complex interplay of psychological and physiological factors. Individuals with PTSD often experience intrusive thoughts, nightmares, hyperarousal, and heightened anxiety related to their traumatic experiences. These symptoms can make it challenging to relax and fall asleep, as the mind remains in a state of heightened alertness. Additionally, the disruption of the body’s stress response system in individuals with PTSD can lead to irregularities in cortisol levels, which play a role in regulating sleep-wake cycles. The chronic activation of the body’s stress response system can further disrupt sleep patterns, creating a cycle of sleep disturbances that exacerbate the symptoms of both PTSD and insomnia.
What are the symptoms of PTSD-related insomnia?
Individuals experiencing PTSD-related insomnia may exhibit a range of symptoms that impact their sleep patterns and overall well-being. Common signs of PTSD-related insomnia include difficulty falling asleep, frequent awakenings during the night, nightmares or vivid dreams related to past traumatic experiences, restless or disrupted sleep, and feelings of fatigue and irritability upon waking. These symptoms can contribute to daytime drowsiness, difficulty concentrating, increased anxiety levels, and a sense of emotional distress. Recognizing these symptoms is crucial in seeking appropriate treatment and support to address the underlying causes of insomnia in the context of post-traumatic stress disorder.
What treatment options are available for PTSD-related insomnia?
There are several treatment options available for PTSD-related insomnia. Cognitive Behavioral Therapy for Insomnia (CBT-I) is a commonly recommended approach that focuses on improving sleep habits and addressing negative thoughts and behaviors that contribute to sleep disturbances. Medications such as sedatives or antidepressants may also be prescribed by healthcare providers to help manage symptoms of insomnia. Additionally, incorporating relaxation techniques, establishing good sleep hygiene practices, and seeking support from mental health professionals who specialize in trauma-informed care can all play a role in effectively treating PTSD-related insomnia. It is important to work closely with healthcare providers to determine the most suitable treatment plan based on individual needs and circumstances.
Is cognitive behavioral therapy effective in treating PTSD-related insomnia?
Cognitive Behavioral Therapy (CBT) has been shown to be an effective treatment for PTSD-related insomnia. CBT targets the negative thought patterns and behaviors that contribute to sleep disturbances, helping individuals develop healthier sleep habits and address underlying issues that disrupt their ability to fall asleep or stay asleep. By focusing on changing these patterns and promoting relaxation techniques, CBT can significantly improve sleep quality for individuals with PTSD, ultimately enhancing their overall well-being and quality of life.
Are there medications specifically for treating insomnia in individuals with PTSD?
Yes, there are medications that can be prescribed to help manage insomnia in individuals with PTSD. Healthcare providers may recommend certain sedatives or antidepressants that have been found to be effective in improving sleep quality and duration. These medications can help address the underlying causes of insomnia, such as anxiety and hyperarousal, and promote better sleep patterns. It is important for individuals with PTSD to consult with a healthcare professional before starting any medication regimen to ensure that the treatment plan is tailored to their specific needs and medical history.
What lifestyle changes can help improve sleep quality for individuals with PTSD?
Making lifestyle changes can significantly improve sleep quality for individuals with PTSD. Establishing a consistent bedtime routine, creating a calm and comfortable sleep environment, and practicing relaxation techniques before bed can all help promote better sleep. Additionally, incorporating regular physical activity into your daily routine, avoiding stimulants like caffeine and alcohol close to bedtime, and maintaining a healthy diet can also contribute to improved sleep quality. It’s important to prioritize self-care and seek support from mental health professionals to develop a comprehensive approach to managing PTSD-related insomnia through lifestyle modifications.
How can relaxation techniques benefit those experiencing PTSD-related insomnia?
Relaxation techniques can significantly benefit individuals experiencing PTSD-related insomnia by helping them calm their minds and bodies before bedtime. Techniques such as deep breathing exercises, progressive muscle relaxation, mindfulness meditation, and guided imagery can promote a sense of relaxation and reduce anxiety and hyperarousal, common symptoms of PTSD. By incorporating these relaxation practices into their bedtime routine, individuals can create a peaceful environment conducive to better sleep. These techniques not only aid in falling asleep but also in staying asleep throughout the night, ultimately improving sleep quality and overall well-being for those struggling with PTSD-related insomnia.
Should individuals seek professional help for managing PTSD-related insomnia?
Seeking professional help for managing PTSD-related insomnia is highly recommended. Individuals experiencing insomnia as a result of PTSD may benefit from the expertise and guidance of mental health professionals who specialize in trauma-informed care. These professionals can provide tailored treatment approaches, such as Cognitive Behavioral Therapy for Insomnia (CBT-I), medication management, relaxation techniques, and sleep hygiene strategies to address the specific challenges associated with PTSD-related sleep disturbances. By seeking professional help, individuals can receive the support they need to improve their sleep quality, manage their symptoms effectively, and work towards healing and recovery from PTSD.