Pain: Understanding and Managing the Unpleasant Sensation
Pain is an inherent part of the human experience. Whether it’s a dull ache, a sharp stab, or a throbbing sensation, pain can be incredibly uncomfortable and disruptive to our daily lives. However, it is important to recognize that pain serves a purpose – it is our body’s way of alerting us to potential harm or injury.
Understanding Pain
Pain can be classified into two main types: acute and chronic. Acute pain is typically short-lived and often associated with an injury or illness. It serves as a warning signal, prompting us to take immediate action to protect ourselves. On the other hand, chronic pain persists for an extended period, usually lasting for more than three months. It can be caused by various factors such as underlying medical conditions or nerve damage.
The Experience of Pain
Pain is subjective and highly individualized. What may be excruciating for one person might be tolerable for another. Factors such as genetics, age, gender, and psychological state can influence how we perceive and respond to pain.
It’s important to note that pain isn’t solely physical; it also has emotional and psychological components. Chronic pain can lead to feelings of frustration, anxiety, depression, and even social isolation. Therefore, addressing the emotional aspect of pain is just as crucial as treating its physical manifestation.
Managing Pain
Fortunately, there are various approaches available for managing pain effectively:
- Medications: Over-the-counter nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen or prescription medications may help alleviate acute or chronic pain by reducing inflammation or blocking pain signals.
- Physical Therapy: Physical therapy techniques such as exercises, stretching, massage therapy, heat/cold therapy, and electrical stimulation can provide relief from certain types of pain while improving mobility and function.
- Psychological Support: Cognitive-behavioral therapy (CBT) and other psychological interventions can help individuals develop coping strategies, manage stress, and change their perception of pain.
- Alternative Therapies: Complementary and alternative therapies like acupuncture, chiropractic care, yoga, meditation, and relaxation techniques have shown promise in reducing pain and promoting overall well-being.
- Lifestyle Changes: Making healthy lifestyle choices such as maintaining a balanced diet, engaging in regular exercise, getting enough sleep, managing stress levels, and avoiding harmful habits like smoking or excessive alcohol consumption can contribute to pain management.
It’s essential to consult with healthcare professionals to determine the most suitable pain management approach for each individual case. A holistic approach that combines multiple strategies often yields the best results.
Empathy and Support
Living with chronic pain can be an isolating experience. It is crucial for friends, family members, and healthcare providers to offer empathy, understanding, and support to individuals dealing with pain. Simple acts of kindness such as listening attentively or offering assistance can make a significant difference in someone’s journey towards pain management.
In conclusion, while pain may be an unpleasant sensation that we would rather avoid altogether, it is a vital aspect of our well-being. Understanding the different types of pain and implementing appropriate management strategies can help individuals regain control over their lives and minimize the impact of pain on their overall quality of life.
9 Frequently Asked Questions About Pain: Causes, Relief, Types, Seriousness, Medications, Natural Remedies, Physical Therapy, Over-the-Counter Safety, and Lifestyle Changes
- What causes pain?
- How can I relieve my pain?
- What are the different types of pain?
- How do I know if my pain is serious?
- What medications are available for managing pain?
- Are there any natural remedies for treating pain?
- Can physical therapy help with chronic pain?
- Is it safe to take over-the-counter medications for pain relief?
- Are there any lifestyle changes that can help reduce the severity of my pain?
What causes pain?
Pain can have various causes, and it often serves as a signal that something is wrong in our bodies. Here are some common factors that can lead to pain:
- Injury or Trauma: Accidents, falls, fractures, sprains, cuts, and burns can all result in acute pain. These injuries typically activate the body’s pain receptors as a protective mechanism.
- Inflammation: Inflammatory conditions such as arthritis, tendinitis, bursitis, or autoimmune disorders like rheumatoid arthritis or lupus can cause persistent pain due to the body’s immune response.
- Nerve Damage: Conditions like neuropathy, nerve compression (such as carpal tunnel syndrome), or injuries to the nerves can lead to chronic pain characterized by tingling, burning sensations, or shooting pains.
- Medical Conditions: Various medical conditions can cause pain as a symptom. Examples include migraines and headaches, fibromyalgia, endometriosis, kidney stones, cancer-related pain, gastrointestinal disorders like gastritis or ulcers, and many others.
- Surgical Procedures: Pain after surgery is common due to tissue damage during the procedure. Post-operative pain management is crucial for ensuring a comfortable recovery.
- Chronic Illnesses: Diseases such as diabetes, multiple sclerosis (MS), HIV/AIDS, or certain types of cancers may cause chronic pain either directly from the condition itself or as a side effect of treatments.
- Psychological Factors: Emotional distress such as stress, anxiety disorders (e.g., generalized anxiety disorder), depression, or unresolved trauma can contribute to the perception of physical pain or amplify existing discomfort.
- Lifestyle Factors: Poor posture and ergonomics at workstations or during physical activities can strain muscles and joints leading to musculoskeletal pain. Additionally, unhealthy habits like smoking or excessive alcohol consumption may exacerbate certain types of pain.
- Aging Process: As we age, degenerative conditions like osteoarthritis or degenerative disc disease become more common, resulting in chronic pain.
It’s important to note that everyone’s experience of pain is unique, and the causes can vary significantly from person to person. Proper evaluation and diagnosis by healthcare professionals are crucial for identifying the underlying cause of pain and developing an appropriate treatment plan.
How can I relieve my pain?
Relieving pain can vary depending on the type and cause of the pain. Here are some general approaches that may help alleviate pain:
- Over-the-counter pain relievers: Non-prescription medications such as acetaminophen (Tylenol) or nonsteroidal anti-inflammatory drugs (NSAIDs) like ibuprofen (Advil, Motrin) can provide temporary relief for mild to moderate pain. However, it’s important to follow the recommended dosage and consult a healthcare professional if you have any underlying health conditions or are taking other medications.
- Heat or cold therapy: Applying heat or cold to the affected area can help reduce pain and inflammation. Heat therapy, such as using a heating pad or taking a warm bath, can relax muscles and increase blood flow to the area. Cold therapy, such as using an ice pack wrapped in a cloth, can numb the area and reduce swelling.
- Physical therapy exercises: Specific exercises recommended by a physical therapist can help strengthen muscles, improve flexibility, and reduce pain associated with certain conditions like back pain or joint problems.
- Relaxation techniques: Techniques such as deep breathing exercises, meditation, guided imagery, or progressive muscle relaxation can help relax both the body and mind, reducing stress and easing pain.
- Massage therapy: Gentle massage or targeted therapeutic massage from a trained professional may help relieve muscle tension and promote relaxation.
- Topical treatments: Over-the-counter creams, gels, or patches containing ingredients like menthol or capsaicin can provide localized relief for muscle or joint pain when applied directly to the affected area.
- Alternative therapies: Some people find relief from alternative therapies such as acupuncture, chiropractic care, herbal remedies, or mind-body practices like yoga or tai chi. It’s important to consult with qualified practitioners in these fields for personalized guidance.
- Proper rest and sleep: Getting enough restful sleep is crucial for managing pain. Establishing a regular sleep routine, creating a comfortable sleep environment, and practicing good sleep hygiene can contribute to pain relief and overall well-being.
- Stress management: Chronic pain can be exacerbated by stress. Engaging in stress-reducing activities like exercise, hobbies, spending time with loved ones, or seeking counseling or therapy can help manage pain more effectively.
- Consult a healthcare professional: If your pain persists or worsens despite self-care measures, it’s important to seek medical advice. A healthcare professional can assess your condition, provide a proper diagnosis, and recommend appropriate treatment options tailored to your specific needs.
Remember that everyone’s experience with pain is unique, and what works for one person may not work for another. It’s essential to listen to your body, be patient with the healing process, and seek professional guidance when needed.
What are the different types of pain?
Pain can be classified into various types based on its characteristics, causes, and duration. Here are some of the different types of pain:
Nociceptive Pain: This type of pain occurs when specialized nerve endings called nociceptors detect potential tissue damage or injury. It can be further divided into two subtypes:
– Somatic Pain: Originating from the skin, muscles, bones, or connective tissues, somatic pain is often described as aching, throbbing, or sharp.
– Visceral Pain: Arising from internal organs such as the abdomen or chest, visceral pain is often described as deep, dull, or cramping.
Neuropathic Pain: Neuropathic pain results from damage or dysfunction in the nervous system itself. It can be caused by conditions like nerve compression, diabetes-related nerve damage (neuropathy), or conditions such as multiple sclerosis or fibromyalgia. Neuropathic pain is often described as burning, shooting, tingling, or electric shocks.
Radicular Pain: Also known as radiculopathy or sciatica when it affects the lower back and legs specifically, radicular pain occurs when a nerve root in the spinal column becomes compressed or irritated. This type of pain often radiates along the path of the affected nerve and may cause numbness and weakness in addition to pain.
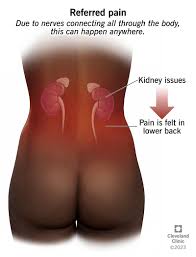
Referred Pain: Referred pain is felt in an area distant from its actual source. For example, during a heart attack, individuals may experience pain radiating down their left arm instead of feeling it directly in their chest.
Phantom Limb Pain: Phantom limb pain occurs after amputation surgery when individuals still perceive sensations and experience pain in the missing limb. The exact cause is not fully understood but may involve changes in the brain’s processing of sensory information.
Psychogenic Pain: Psychogenic pain is pain that is primarily caused or influenced by psychological factors such as stress, anxiety, or depression. It may manifest as headaches, back pain, or generalized body pain.
Acute Pain: Acute pain is temporary and typically occurs due to an injury, surgery, or illness. It serves as a warning signal and usually subsides as the underlying cause heals.
Chronic Pain: Chronic pain persists for an extended period, often lasting beyond three months. It may result from conditions like arthritis, fibromyalgia, or nerve damage. Chronic pain can significantly impact daily life and requires long-term management.
It’s important to note that individuals may experience a combination of different types of pain simultaneously. Proper diagnosis and evaluation by healthcare professionals can help determine the specific type of pain and guide appropriate treatment approaches.
How do I know if my pain is serious?
Determining the seriousness of pain can be challenging, as it varies from person to person and depends on various factors. However, there are certain signs and symptoms that may indicate the need for immediate medical attention. Here are some guidelines to consider:
- Intensity of Pain: Severe or excruciating pain that is sudden and unrelenting may warrant immediate medical attention. If the pain is unbearable and significantly affects your ability to function or perform daily activities, it is advisable to seek medical help.
- Duration of Pain: If your pain persists for an extended period or becomes chronic (lasting more than three months), it is recommended to consult a healthcare professional. Chronic pain may be indicative of an underlying condition that requires evaluation and treatment.
- Changes in Pain Pattern: Pay attention if your pain changes in intensity, location, or character over time. For example, if you experience a sudden increase in severity or notice new symptoms accompanying the pain, it could be a sign of a more serious condition.
- Associated Symptoms: Take note of any additional symptoms accompanying your pain. Symptoms such as fever, unexplained weight loss, swelling, numbness or tingling, difficulty breathing, chest pain, dizziness, or loss of consciousness should not be ignored and should prompt immediate medical attention.
- Trauma or Injury: If your pain is a result of an accident, fall, significant trauma, or injury, it is crucial to seek medical evaluation promptly. In such cases, there may be underlying damage that requires immediate attention.
- Pre-existing Medical Conditions: If you have pre-existing medical conditions such as heart disease, diabetes, cancer, or any other chronic illness and experience new or worsening pain related to these conditions, it is important to consult with your healthcare provider for appropriate assessment and management.
- Gut Feeling: Trust your instincts when it comes to assessing the seriousness of your pain. If you have concerns about the intensity, duration, or any other aspect of your pain, it is always better to err on the side of caution and seek professional medical advice.
Remember, this guidance is not a substitute for professional medical advice. If you are unsure about the seriousness of your pain or have any concerns, it is best to consult with a healthcare professional who can evaluate your specific situation and provide appropriate guidance and treatment.
What medications are available for managing pain?
There are several medications available for managing pain, ranging from over-the-counter options to prescription drugs. The choice of medication depends on the type and severity of pain, as well as individual circumstances. It is important to consult with a healthcare professional to determine the most appropriate medication for your specific situation. Here are some commonly used pain medications:
- Nonsteroidal Anti-Inflammatory Drugs (NSAIDs): These include medications like ibuprofen (Advil, Motrin) and naproxen (Aleve). NSAIDs work by reducing inflammation, which can help relieve pain associated with conditions such as arthritis, muscle strains, and menstrual cramps.
- Acetaminophen: Commonly known as Tylenol, acetaminophen is an over-the-counter medication that can provide relief for mild to moderate pain. It is not an anti-inflammatory drug but can help reduce fever and alleviate headaches, toothaches, and general body aches.
- Opioids: Prescription opioids are powerful pain relievers that work by binding to opioid receptors in the brain and blocking pain signals. They are typically reserved for severe acute pain or chronic pain that does not respond to other treatments. Examples include codeine, oxycodone (OxyContin), hydrocodone (Vicodin), and morphine.
- Antidepressants: Certain antidepressant medications, such as tricyclic antidepressants (TCAs) or selective serotonin-norepinephrine reuptake inhibitors (SNRIs), may be prescribed for chronic pain management. These medications can help regulate neurotransmitters in the brain and modify how the body perceives pain.
- Anticonvulsants: Medications typically used to treat seizures or epilepsy, such as gabapentin (Neurontin) or pregabalin (Lyrica), have also shown effectiveness in managing certain types of chronic neuropathic pain.
- Topical Analgesics: These are creams, gels, or patches that can be applied directly to the skin over the painful area. They work by numbing the skin or reducing inflammation locally. Examples include lidocaine patches and capsaicin creams.
It is important to note that all medications have potential side effects and risks. It is crucial to follow the prescribed dosage and consult with a healthcare professional to ensure safe and appropriate use of any pain medication.
Are there any natural remedies for treating pain?
Yes, there are several natural remedies that can help alleviate pain. While it’s important to note that natural remedies may not work for everyone or in all situations, they can provide relief for certain types of pain. Here are some commonly used natural remedies:
- Herbal Supplements: Certain herbs have analgesic and anti-inflammatory properties that can help reduce pain. Examples include turmeric, ginger, boswellia, and devil’s claw. These herbs can be taken as supplements or used in cooking.
- Essential Oils: Essential oils derived from plants such as lavender, peppermint, eucalyptus, and chamomile have soothing properties and can be helpful in relieving pain. They can be applied topically (diluted with a carrier oil) or diffused into the air.
- Heat and Cold Therapy: Applying heat or cold to the affected area can provide temporary relief from pain. A warm compress or heating pad helps relax muscles and increase blood flow, while an ice pack numbs the area and reduces inflammation.
- Acupuncture: This ancient Chinese practice involves inserting thin needles into specific points on the body to stimulate energy flow and promote pain relief. Acupuncture has been found effective in managing various types of pain.
- Exercise and Stretching: Engaging in regular physical activity and stretching exercises helps improve flexibility, strengthen muscles, and reduce pain associated with conditions like arthritis or muscle strains.
- Mind-Body Techniques: Practices such as meditation, deep breathing exercises, guided imagery, and progressive muscle relaxation can help manage pain by promoting relaxation, reducing stress levels, and redirecting focus away from discomfort.
- Dietary Changes: Incorporating an anti-inflammatory diet rich in fruits, vegetables, whole grains, lean proteins (such as fish), healthy fats (like olive oil), and avoiding processed foods may help reduce inflammation-related pain.
It’s important to consult with a healthcare professional before trying any natural remedies, especially if you have an underlying medical condition or are taking medications. They can provide guidance on the appropriate use and potential interactions with other treatments.
Can physical therapy help with chronic pain?
Yes, physical therapy can be an effective treatment option for managing chronic pain. Physical therapists are trained healthcare professionals who specialize in assessing and treating musculoskeletal conditions, including chronic pain. They work closely with patients to develop personalized treatment plans that address the underlying causes of pain and improve physical function.
Here are some ways in which physical therapy can help with chronic pain:
- Pain Reduction: Physical therapists use various techniques such as manual therapy, therapeutic exercises, and modalities like heat or cold therapy to reduce pain levels. These interventions can help alleviate muscle tension, improve joint mobility, and promote relaxation.
- Improved Function and Mobility: Chronic pain often limits a person’s ability to perform daily activities or move freely. Physical therapists focus on restoring functional abilities by targeting specific areas of weakness or stiffness through exercises and stretches. They may also provide assistive devices or recommend modifications to aid in movement.
- Education and Self-Management: Physical therapists educate patients about their condition, teaching them strategies for self-management and pain relief. This may include advice on posture, body mechanics, ergonomics, and techniques for managing flare-ups or exacerbations of pain.
- Rehabilitation after Injury or Surgery: In cases where chronic pain stems from a previous injury or surgery, physical therapy plays a crucial role in rehabilitation. Therapists guide patients through progressive exercises and therapies to regain strength, flexibility, and range of motion while minimizing pain.
- Mind-Body Approaches: Physical therapists may incorporate mind-body techniques such as relaxation exercises, breathing techniques, mindfulness-based practices, or biofeedback to help patients manage stress levels and improve their overall well-being.
It is important to note that every individual’s experience with chronic pain is unique; therefore, the treatment approach should be tailored to their specific needs. Physical therapy is often utilized as part of a comprehensive multidisciplinary approach that may involve other healthcare providers such as physicians, psychologists, occupational therapists, and pain management specialists.
If you are experiencing chronic pain, consulting with a physical therapist can be beneficial in developing an individualized treatment plan to address your specific condition and goals.
Is it safe to take over-the-counter medications for pain relief?
Over-the-counter (OTC) medications for pain relief can be safe and effective when used as directed. However, it is important to follow the recommended dosage and guidelines provided by the manufacturer or healthcare professional. Here are a few key points to consider:
- Read and Follow Instructions: Always read the label and instructions before taking any medication. Pay attention to the recommended dosage, frequency, and any precautions or warnings.
- Know Your Medications: Different OTC pain relievers contain different active ingredients, such as acetaminophen, ibuprofen, or aspirin. Understand which ingredient is present in the medication you are taking, as well as its potential side effects or interactions with other medications you may be taking.
- Consider Your Health Conditions: Certain health conditions or medical history may require specific precautions or contraindications when taking OTC pain relievers. Consult with a healthcare professional if you have any underlying health conditions such as liver disease, kidney problems, stomach ulcers, or allergies.
- Avoid Overuse: Taking more than the recommended dosage of OTC pain medications can lead to adverse effects and potential harm. It’s important to follow the specified dosing instructions and not exceed the maximum daily dose.
- Be Aware of Potential Side Effects: OTC pain relievers may cause side effects such as stomach upset, dizziness, drowsiness, or allergic reactions in some individuals. If you experience any unusual symptoms after taking a medication, discontinue use and consult a healthcare professional.
- Seek Professional Advice: If you have persistent or severe pain that does not improve with OTC medications or if you are unsure about which medication is suitable for your condition, it is advisable to consult with a healthcare professional for proper diagnosis and guidance.
Remember that while OTC pain relievers can provide temporary relief for mild to moderate pain, they may not address the underlying cause of your pain. If your pain persists or worsens, it is essential to seek medical advice for a comprehensive evaluation and appropriate treatment.
Are there any lifestyle changes that can help reduce the severity of my pain?
Yes, there are lifestyle changes that can help reduce the severity of pain. While these changes may not eliminate pain entirely, they can contribute to better pain management and improve overall well-being. Here are some lifestyle modifications that may be beneficial:
- Regular Exercise: Engaging in low-impact exercises like walking, swimming, or cycling can help strengthen muscles, improve flexibility, and release endorphins, which are natural pain-relieving chemicals in the body.
- Balanced Diet: Adopting a nutritious diet can support overall health and potentially reduce inflammation in the body. Include foods rich in antioxidants (fruits and vegetables), omega-3 fatty acids (fish, nuts, and seeds), and whole grains while minimizing processed foods and sugary snacks.
- Stress Management: Chronic stress can exacerbate pain symptoms. Incorporate stress-reducing techniques such as deep breathing exercises, meditation, yoga, or engaging in hobbies to promote relaxation and emotional well-being.
- Adequate Sleep: Prioritize getting enough restful sleep as it plays a crucial role in pain management. Establish a consistent sleep schedule, create a relaxing bedtime routine, ensure a comfortable sleep environment, and limit caffeine intake.
- Posture and Ergonomics: Maintain good posture while sitting and standing to prevent unnecessary strain on joints and muscles. Use ergonomic tools or make adjustments to your work environment to minimize discomfort during daily activities.
- Weight Management: Maintaining a healthy weight reduces stress on joints and can alleviate pain associated with conditions such as arthritis or back problems.
- Avoid Harmful Habits: Smoking tobacco products can worsen certain types of pain by impairing circulation and healing processes. Limit alcohol consumption as it can interfere with sleep quality and increase sensitivity to pain.
Remember that everyone’s experience with pain is unique, so it’s essential to consult with healthcare professionals for personalized advice tailored to your specific condition or situation. They can provide guidance on lifestyle modifications and additional pain management strategies that may be most beneficial for you.